Items filtered by date: March 2025
Do Your Child's Feet Hurt?
How to Properly Care for Your Feet

Taking care of your feet is essential for overall health and mobility. Washing them daily with warm water and mild soap helps prevent infections and removes dirt and sweat buildup. Moisturizing regularly keeps the skin soft and prevents dryness or cracking. Wearing properly fitted shoes with adequate support reduces pressure on the feet and minimizes discomfort. Proper toenail trimming is also important, as cutting nails straight across and avoiding cutting them too short helps prevent ingrown toenails. Regularly inspecting the feet for any cuts, blisters, or changes in skin texture can help detect potential problems early. Additionally, stretching and strengthening exercises improve circulation and foot flexibility. If you have developed any type of foot condition, it is suggested that you promptly contact a podiatrist who can offer effective treatment solutions, and guide you on additional everyday foot care tips.
Everyday foot care is very important to prevent infection and other foot ailments. If you need your feet checked, contact Dr. Michael A. Wood from Foot Health Institute. Our doctor can provide the care you need to keep you pain-free and on your feet.
Everyday Foot Care
Often, people take care of their bodies, face and hair more so than they do for their feet. But the feet are a very important aspect of our bodies, and one that we should pay more attention to. Without our feet, we would not be able to perform most daily tasks.
It is best to check your feet regularly to make sure there are no new bruises or cuts that you may not have noticed before. For dry feet, moisturizer can easily be a remedy and can be applied as often as necessary to the affected areas. Wearing shoes that fit well can also help you maintain good foot health, as well as making it easier to walk and do daily activities without the stress or pain of ill-fitting shoes, high heels, or even flip flops. Wearing clean socks with closed shoes is important to ensure that sweat and bacteria do not accumulate within the shoe. Clean socks help to prevent Athlete’s foot, fungi problems, bad odors, and can absorb sweat.
If you have any questions please feel free to contact one of our offices located in Lansing, and Chicago, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
When Your Toenails Start Changing

Toenail fungus does not appear overnight, but once it takes hold, it is hard to ignore. At first, a small white or yellow spot may appear on the toenail. Over time, the nail thickens, turns yellow or brown, and may become brittle, crumbly, or even lift from the nail bed. Some people experience a foul odor, while others feel discomfort when wearing shoes. Treatment takes patience. Mild cases may improve with antifungal creams or medicated nail lacquers, but more stubborn infections often require prescription oral medication or laser treatments. In severe cases, the nail may need to be removed. Prevention is key. Keep feet clean and dry, wear breathable shoes, and avoid walking barefoot in public places like around pools or in locker rooms. Trim nails straight across and disinfect nail clippers. If the infection persists, it is suggested that you see a podiatrist who can recommend the best course of action.
For more information about treatment, contact Dr. Michael A. Wood of Foot Health Institute. Our doctor can provide the care you need to keep you pain-free and on your feet.
Toenail Fungus Treatment
Toenail fungus is a condition that affects many people and can be especially hard to get rid of. Fortunately, there are several methods to go about treating and avoiding it.
Antifungals & Deterrence
Oral antifungal medicine has been shown to be effective in many cases. It is important to consult with a podiatrist to determine the proper regiment for you, or potentially explore other options.
Applying foot powder on the feet and shoes helps keep the feet free of moisture and sweat.
Sandals or open toed shoes – Wearing these will allow air movement and help keep feet dry. They also expose your feet to light, which fungus cannot tolerate. Socks with moisture wicking material also help as well.
If you have any questions please feel free to contact one of our offices located in Lansing, and Chicago, IL . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
When Your Toenails Start Changing

Toenail fungus does not appear overnight, but once it takes hold, it is hard to ignore. At first, a small white or yellow spot may appear on the toenail. Over time, the nail thickens, turns yellow or brown, and may become brittle, crumbly, or even lift from the nail bed. Some people experience a foul odor, while others feel discomfort when wearing shoes. Treatment takes patience. Mild cases may improve with antifungal creams or medicated nail lacquers, but more stubborn infections often require prescription oral medication or laser treatments. In severe cases, the nail may need to be removed. Prevention is key. Keep feet clean and dry, wear breathable shoes, and avoid walking barefoot in public places like around pools or in locker rooms. Trim nails straight across and disinfect nail clippers. If the infection persists, it is suggested that you see a podiatrist who can recommend the best course of action.
For more information about treatment, contact Dr. Michael A. Wood of Foot Health Institute. Our doctor can provide the care you need to keep you pain-free and on your feet.
Toenail Fungus Treatment
Toenail fungus is a condition that affects many people and can be especially hard to get rid of. Fortunately, there are several methods to go about treating and avoiding it.
Antifungals & Deterrence
Oral antifungal medicine has been shown to be effective in many cases. It is important to consult with a podiatrist to determine the proper regiment for you, or potentially explore other options.
Applying foot powder on the feet and shoes helps keep the feet free of moisture and sweat.
Sandals or open toed shoes – Wearing these will allow air movement and help keep feet dry. They also expose your feet to light, which fungus cannot tolerate. Socks with moisture wicking material also help as well.
If you have any questions please feel free to contact one of our offices located in Lansing, and Chicago, IL . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Painful Plantar Fasciitis

Plantar fasciitis is perhaps the most common cause of heel pain. It results from inflammation of the thick band of tissue called the plantar fascia, that runs along the bottom of the foot. The primary symptom is sharp, stabbing pain in the heel, particularly when taking your first steps in the morning or after sitting for a while. The pain can lessen with movement but may return after long periods of standing or walking. This condition is often caused by repetitive strain on the plantar fascia, which can be triggered by activities like running, wearing improper footwear, or having flat feet or high arches. A podiatrist can diagnose plantar fasciitis through a physical exam and may use imaging tests for a clearer view. Treatment typically involves stretching exercises, custom orthotics, and anti-inflammatory medication. In more severe cases, corticosteroid injections may be recommended. If you are dealing with this condition, it is suggested that you schedule an appointment with a podiatrist for proper care and relief.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Dr. Michael A. Wood from Foot Health Institute. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact one of our offices located in Lansing, and Chicago, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Painful Plantar Fasciitis

Plantar fasciitis is perhaps the most common cause of heel pain. It results from inflammation of the thick band of tissue called the plantar fascia, that runs along the bottom of the foot. The primary symptom is sharp, stabbing pain in the heel, particularly when taking your first steps in the morning or after sitting for a while. The pain can lessen with movement but may return after long periods of standing or walking. This condition is often caused by repetitive strain on the plantar fascia, which can be triggered by activities like running, wearing improper footwear, or having flat feet or high arches. A podiatrist can diagnose plantar fasciitis through a physical exam and may use imaging tests for a clearer view. Treatment typically involves stretching exercises, custom orthotics, and anti-inflammatory medication. In more severe cases, corticosteroid injections may be recommended. If you are dealing with this condition, it is suggested that you schedule an appointment with a podiatrist for proper care and relief.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Dr. Michael A. Wood from Foot Health Institute. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact one of our offices located in Lansing, and Chicago, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
How to Manage the Onset of Flat Feet
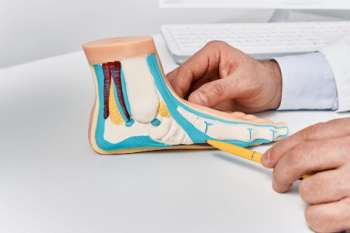
Progressive collapsing foot deformity, also known as adult-acquired flatfoot, occurs when the arch gradually collapses, leading to changes in your foot’s shape and function. Adult-acquired flatfoot often results from dysfunction in the posterior tibial tendon, which plays a key role in supporting the arch and turning the foot inward. As this tendon weakens, the foot may flatten, and the alignment of the ankle can shift, sometimes causing pain or difficulty walking. Aging, previous injuries, obesity, diabetes, or arthritis may contribute to the development of adult-acquired flatfoot. It may result in pain along the inside of the ankle, swelling, or an outward shift of the foot’s position. A podiatrist can assess the severity of the condition using certain imaging tests to determine the best course of treatment. Supportive devices, orthotic inserts, and in more advanced cases, surgery, may help restore function and relieve pain. If you notice that your feet have become flatter, it is suggested that you schedule an appointment with a podiatrist for an exam, diagnosis, and treatment options.
Flatfoot is a condition many people suffer from. If you have flat feet, contact Dr. Michael A. Wood from Foot Health Institute. Our doctor will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
- Pain around the heel or arch area
- Trouble standing on the tip toe
- Swelling around the inside of the ankle
- Flat look to one or both feet
- Having your shoes feel uneven when worn
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions please feel free to contact one of our offices located in Lansing, and Chicago, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
How to Manage the Onset of Flat Feet
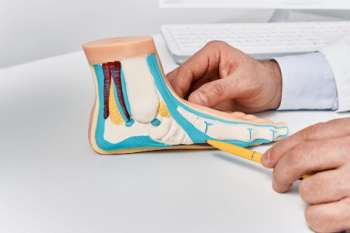
Progressive collapsing foot deformity, also known as adult-acquired flatfoot, occurs when the arch gradually collapses, leading to changes in your foot’s shape and function. Adult-acquired flatfoot often results from dysfunction in the posterior tibial tendon, which plays a key role in supporting the arch and turning the foot inward. As this tendon weakens, the foot may flatten, and the alignment of the ankle can shift, sometimes causing pain or difficulty walking. Aging, previous injuries, obesity, diabetes, or arthritis may contribute to the development of adult-acquired flatfoot. It may result in pain along the inside of the ankle, swelling, or an outward shift of the foot’s position. A podiatrist can assess the severity of the condition using certain imaging tests to determine the best course of treatment. Supportive devices, orthotic inserts, and in more advanced cases, surgery, may help restore function and relieve pain. If you notice that your feet have become flatter, it is suggested that you schedule an appointment with a podiatrist for an exam, diagnosis, and treatment options.
Flatfoot is a condition many people suffer from. If you have flat feet, contact Dr. Michael A. Wood from Foot Health Institute. Our doctor will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
- Pain around the heel or arch area
- Trouble standing on the tip toe
- Swelling around the inside of the ankle
- Flat look to one or both feet
- Having your shoes feel uneven when worn
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions please feel free to contact one of our offices located in Lansing, and Chicago, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.